Client Resources
Insurance and Fees
We are in network with CareFirst/BCBS. We are out of network with all other insurance companies. We can provide monthly superbills of appointments to share with an insurance company if needed. All clients have the option of paying out-of-pocket without going through any insurance company at all. This means paying the full cost of the session up-front at the rates listed below.
*There are some significant benefits to opting out of the insurance system for therapy. Paying out of pocket means that there is no requirement that diagnostic criteria is met in order for treatment to be covered. Mental health diagnoses can feel stigmatizing to some and the practice of diagnosis is seen by many as antithetical to holistic assessment and treatment. Paying out of pocket also allows the provider and the client to hold absolute decision-making power over how often and how long a client attends therapy as well as what modalities are most effective for each individual client.*
Depending on the insurance plan, the amount owed for sessions can range from close to the full cost if there is a deductible for mental health (often ranging from $100-$117), a copay (a flat fee for the session cost, usually ranging from $10-$50 a session), or a coinsurance (a percentage of the session cost, usually ranging from $10-$50 session).
If using insurance, the out-of-pocket cost will depend on the client’s individual plan. Deductibles and copays/coinsurance will vary. If not using insurance, the self-pay rates can be found below in the pricing section.
EOBs (Explanation of Benefits) can usually be found in the insurance member portal or by calling the member services on the insurance card.
We recommend that clients ask the following questions to their insurance provider to help determine their benefits:
- Does my health insurance plan include mental health benefits?
- Do I have a deductible? If so, what is it and have I met it yet?
- Does my plan limit how many sessions per calendar year I can have? If so, what is the limit?
- Does my plan require a preauthorization or referral from a primary care provider in order for my services to be covered?
Copays or deductible costs should be paid on the day of the therapy session. This policy has some flexibility on a case by case basis that needs to be discussed with the therapist in advance.
Current Pricing
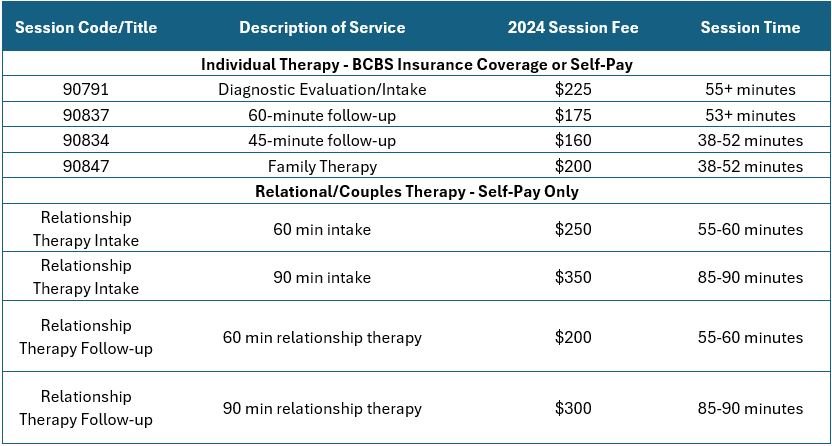
For folks using their BCBS insurance coverage, copays or coinsurance are set through the insurance provider. For clients who are seeking relational/couples therapy or are wanting to self-pay for individual therapy, the below rates are current through the end of 2024. It is important to note that self-pay pricing will increase a small percentage each year to account for increases in operation costs.
Cancellation & No-Show Policy
We know that life happens and sometimes unexpected schedule conflicts come up. We also recognize the importance of setting healthy and transparent boundaries and of holding ourselves accountable. We ask that clients email or text their clinician to cancel with at least 24 hours notice from the scheduled appointment time. We consider a session no-show one in which a client has not logged in to the virtual meeting room and/or notified the therapist of a brief delay by 10 minutes after the start of the scheduled session time.
Under Constellation Counseling’s grace policy, clients receive one free late cancellation and one free no-show per calendar year. Beyond this, should the need to reschedule with less than 24 hours notice come up, at the therapist’s discretion, rescheduling the session within the week may be possible without being charged the late cancellation fee. A session no-show will not be rescheduled within the week and will be charged the full no-show fee in most situations.
Cancellation/no-show fee is equal to the full self-pay rate of the scheduled session type; late cancellations and no shows are not covered by insurance
Good Faith Estimate
As of January 1, 2022, under Section 2799B-6 of the Public Health Service Act, health care providers and health care facilities are required to inform individuals who are not enrolled in a plan or coverage or a Federal health care program, or not seeking to file a claim with their plan or coverage both orally and in writing of their ability, upon request or at the time of scheduling health care items and services, to receive a “Good Faith Estimate” of expected charges.
You have the right to receive a “Good Faith Estimate” explaining how much your medical care will cost.
Under the law, health care providers need to give patients who don’t have insurance or who are not using insurance an estimate of the bill for medical items and services.
You have the right to receive a Good Faith Estimate for the total expected cost of any non-emergency items or services. This includes related costs like medical tests, prescription drugs, equipment, and hospital fees.
Make sure your health care provider gives you a Good Faith Estimate in writing at least 1 business day before your medical service or item. You can also ask your health care provider, and any other provider you choose, for a Good Faith Estimate before you schedule an item or service.
If you receive a bill that is at least $400 more than your Good Faith Estimate, you can dispute the bill.
Make sure to save a copy or picture of your Good Faith Estimate. For questions or more information about your right to a Good Faith Estimate, visit www.cms.gov/nosurprises.